Vitamin D overview

Contents
What is a vitamin D test? What does a vitamin D test measure? What does your vitamin D score mean? What factors impact vitamin D test results? Groups at risk for low vitamin D levels Diet and lifestyle strategies shown to improve vitamin D test results Supplements used to improve vitamin D test resultsWhat is a vitamin D test?
A vitamin D test measures the amount of 25-hydroxyvitamin D in your blood and is used to assess vitamin D status. Vitamin D is a fat-soluble vitamin that plays important roles in bone health, calcium absorption, blood sugar regulation, immunity (particularly in regards to COVID-19), and may even protect against some cancers.
What does a vitamin D test measure?
A vitamin D test measures the level of 25-hydroxyvitamin D, also known as 25(OH)D, in your blood. Your liver and kidneys convert dietary vitamin D2 and vitamin D3 into 25(OH)D.
Vitamin D2 is mostly obtained from the diet through fortified foods like breakfast cereal, milk, and yogurt. Vitamin D3 is made by your body from cholesterol and exposure to sunlight (UVB rays) but is also found in eggs and certain fatty fish.
What does your vitamin D score mean?
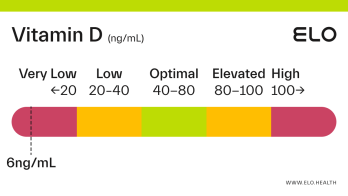
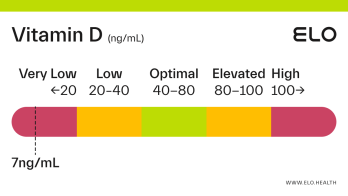
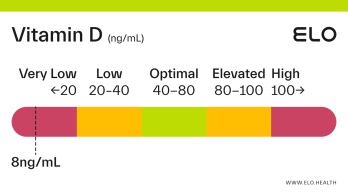
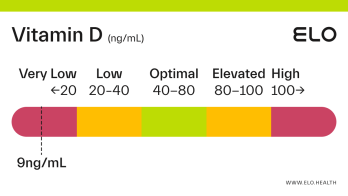
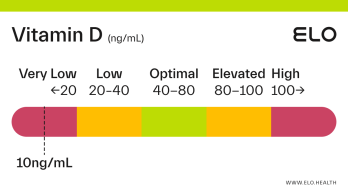
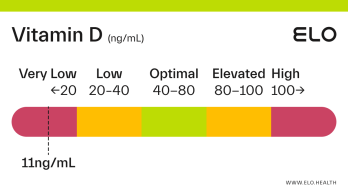
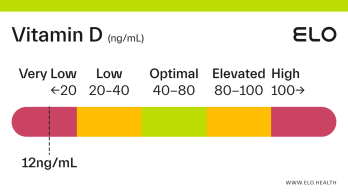
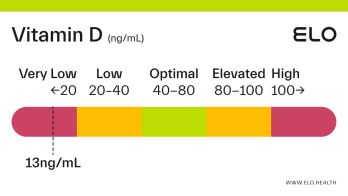
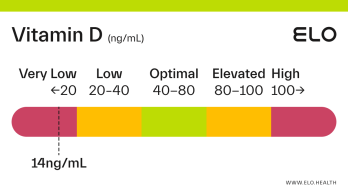
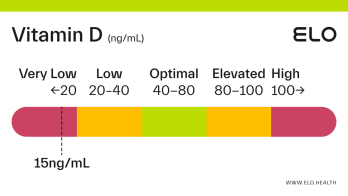
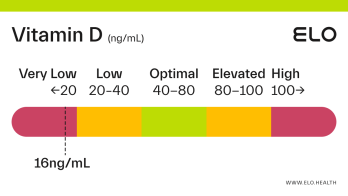
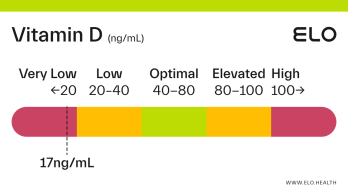
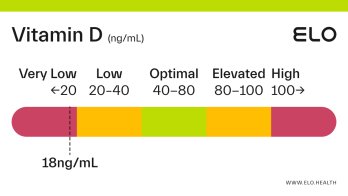
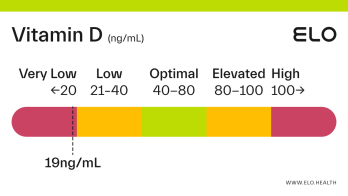
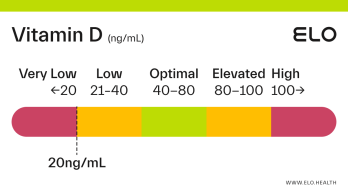
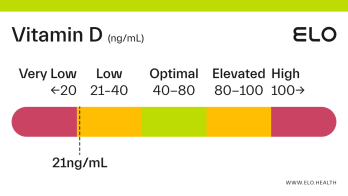
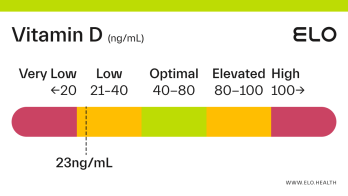
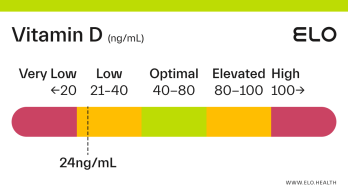
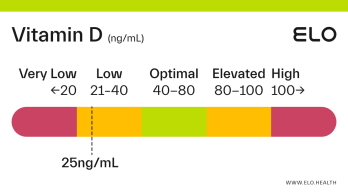
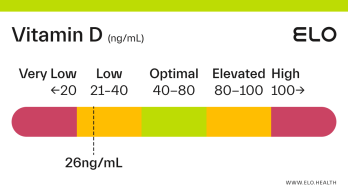
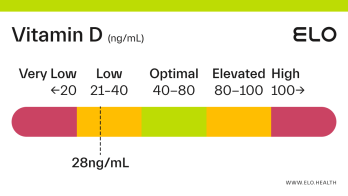
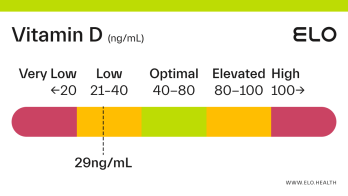
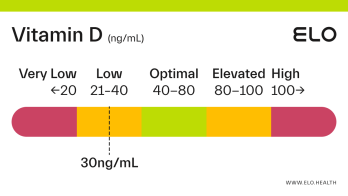
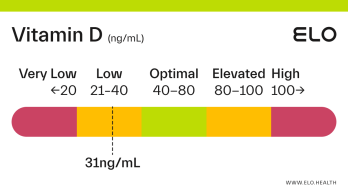
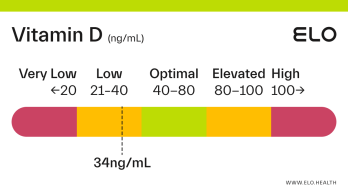
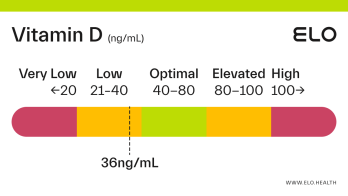
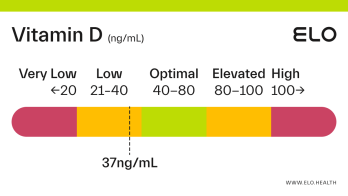
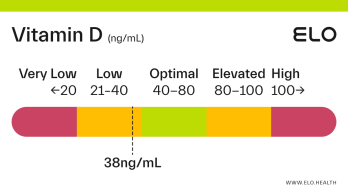
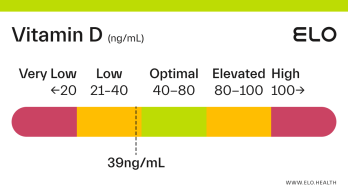
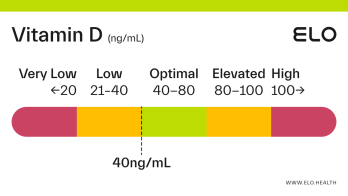
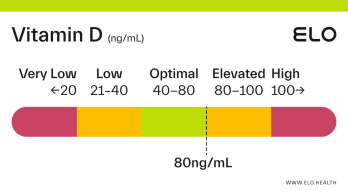
Based on a thorough review of the research, we classify vitamin D status as follows at Elo:
Very low: <20 ng/mL
Low: 20-40 ng/mL
Optimal: 40-80 ng/mL
Elevated: 80-100 ng/mL
High:
>
100 ng/mL
Very low vitamin D
If your vitamin D level is <20 ng/mL you are likely vitamin D deficient. Deficiency can occur from inadequate dietary intake, limited exposure to sunlight, if the kidneys cannot convert 25(OH)D to its active form, or if absorption of vitamin D is inadequate. Vitamin D deficiency in adults is associated with a condition called osteomalacia which weakens bones over time.
Low vitamin D may also put you at increased risk for, and severity of COVID-19, diabetes, and cancer. It may also increase your risk for certain autoimmune and neurodegenerative diseases including multiple sclerosis and Alzheimer’s.
COVID-19: Early research suggests having optimal vitamin D levels may lower your risk for COVID-19 infection and severity [4].
Type 2 diabetes: Vitamin D plays a role in insulin production and sensitivity. Research shows there is a clear association between low vitamin D levels in patients with insulin resistance and a high risk of developing type 2 diabetes [5].
Cancer: Current evidence seems to suggest higher vitamin D levels may be beneficial for those diagnosed with cancer. One meta-analysis found overall survival from colorectal cancer, lung cancer, and lymphoma was greater in people with higher blood levels of vitamin D. There may also be a modest benefit for vitamin D supplementation during treatment [6].
Autoimmune diseases: Vitamin D plays a role in prevention and protection from autoimmune diseases, including multiple sclerosis, type 1 diabetes, and systemic lupus erythematosus (SLE, the most common type of lupus) [7].
Neurodegenerative diseases: An increasing number of studies indicate that vitamin D deficiency is associated with a wide range of neuropsychiatric disorders and neurodegenerative diseases including depression, Alzheimer’s, and Parkinson’s [8].
Low vitamin D
Vitamin D levels from 20-40 ng/mL are considered low or inadequate. If you fall in this range, you likely do not have an adequate amount of vitamin D for optimal bone and overall health.
Optimal vitamin D
Optimal vitamin D levels are between 40-80 ng/mL. This means your body has adequate amounts of vitamin D to support bone health, neuromuscular and immune function, glucose metabolism, and more.
Elevated vitamin D
You have elevated vitamin D if your level is >80 ng/mL. However, adverse effects are typically only observed at levels >125 ng/mL.
High vitamin D
Vitamin D levels >100 ng/mL are considered high. Vitamin D toxicity can have adverse effects, including hypercalcemia, a buildup of calcium in the blood. The good news is you cannot reach dangerously high blood levels through diet and sun exposure alone. Vitamin D toxicity is rare and occurs almost exclusively as a result of unmonitored, long-term, high-dose supplementation.
What factors impact vitamin D test results?
Factors that impact vitamin D levels include:
Where you live and the amount of sun exposure you get (people who live at latitudes above 37°N can’t synthesize vitamin D year-round)
Your skin color (the darker your skin, the more sun exposure is needed to produce adequate amounts)
Dietary intake of vitamin D
Age (aging reduces vitamin D production in skin)
Pregnancy & breastfeeding
Diseases that may impede absorption (Cystic fibrosis, Chron’s, and celiac) or synthesis of vitamin D (kidney and liver disease)
Obesity (high body fat sequesters vitamin D)
Reduced absorption related to weight loss surgery
Certain medications including laxatives, steroids, and cholesterol-lowering drugs
Sun protection (increases your likelihood for low vitamin D)
Groups at risk for low vitamin D levels
Elderly (partly due to a decline in the skin’s ability to synthesize vitamin D with age)
Dark complexion
Cold or northern climates (people who live above 37°N latitude cannot synthesize vitamin D year-round)
Limited sun exposure (such as those who spend the majority of their time indoors or are covered when outside)
Women who are pregnant and/or breastfeeding
Cystic fibrosis, Chrohn’s, celiac, kidney, and liver disease, or other conditions that interfere with vitamin D absorption or synthesis
Obese individuals or those who have had gastric bypass surgery
Diet and lifestyle strategies shown to improve vitamin D test results
Consume vitamin D-rich foods regularly (at least 600 IU daily) paired with a source of fat for improved absorption. The best sources of dietary vitamin D include fatty fish (trout, salmon, tuna, and mackerel), as well as fortified dairy/dairy alternatives, egg yolks, and mushrooms.
Get 10–30 minutes of unprotected midday sunlight most days of the week. Our bodies synthesize vitamin D naturally when exposed to ultraviolet light. However, this alone is not sufficient to maintain optimal vitamin D levels.
Take a vitamin D supplement
Supplements used to improve vitamin D test results
If your vitamin D levels are low, a daily vitamin D supplement can help you get into the optimal range. The ideal dose of vitamin D depends on your current vitamin D level and how often you supplement.
To achieve or maintain adequate body stores of vitamin D, moderate daily supplementation of vitamin D3 1,000-5,000IU (cholecalciferol) should be considered if levels are at or below 40 ng/mL.
References
National Institutes of Health. (2021, March 26). Office of Dietary Supplements - Vitamin D. National Institutes of Health – Office of Dietary Supplements.
https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Alshahrani, F., & Aljohani, N. (2013). Vitamin D: deficiency, sufficiency, and toxicity. Nutrients, 5(9), 3605–3616.
https://doi.org/10.3390/nu5093605
Holick M. F. (2009). Vitamin D status: measurement, interpretation, and clinical application. Annals of epidemiology, 19(2), 73–78.
https://doi.org/10.1016/j.annepidem.2007.12.001
Demir, M., Demir, F., & Aygun, H. (2021). Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. Journal of medical virology, 93(5), 2992–2999.
https://doi.org/10.1002/jmv.26832
Kayaniyil, S., Vieth, R., Retnakaran, R., Knight, J. A., Qi, Y., Gerstein, H. C., Perkins, B. A., Harris, S. B., Zinman, B., & Hanley, A. J. (2010). Association of vitamin D with insulin resistance and beta-cell dysfunction in subjects at risk for type 2 diabetes. Diabetes care, 33(6), 1379–1381.
https://doi.org/10.2337/dc09-2321
Examine.com. (2019, April). A D-fence against cancer?
https://examine.com/members/deep-dives/article/a-d-fence-against-cancer/
Yang, C. Y., Leung, P. S., Adamopoulos, I. E., & Gershwin, M. E. (2013). The implication of vitamin D and autoimmunity: a comprehensive review. Clinical reviews in allergy & immunology, 45(2), 217–226.
https://doi.org/10.1007/s12016-013-8361-3
Groves, N. J., McGrath, J. J., & Burne, T. H. (2014). Vitamin D as a neurosteroid affecting the developing and adult brain. Annual review of nutrition, 34, 117–141.
https://doi.org/10.1146/annurev-nutr-071813-105557