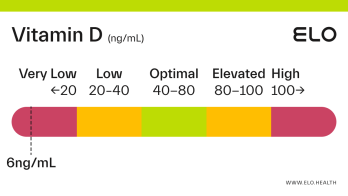
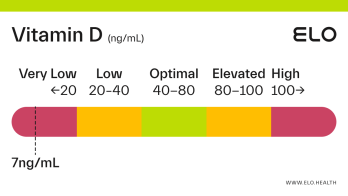
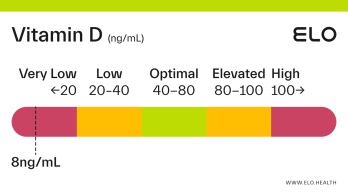
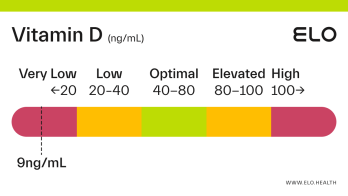
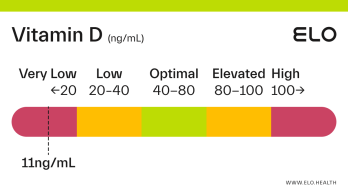
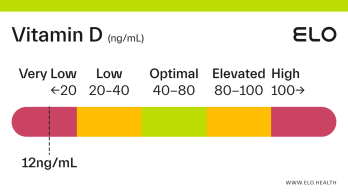
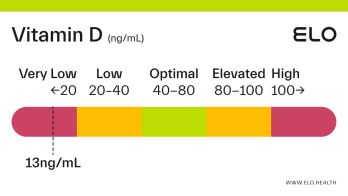
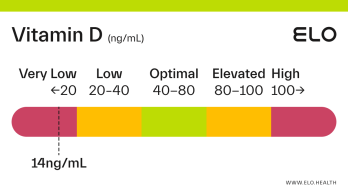
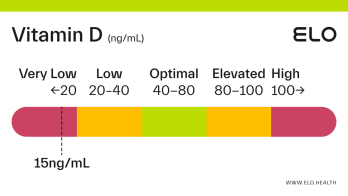
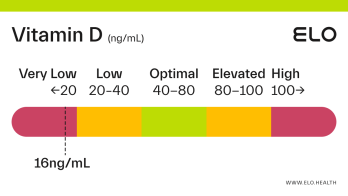
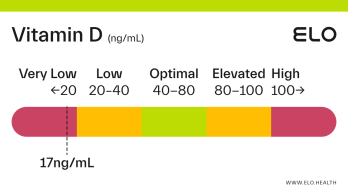
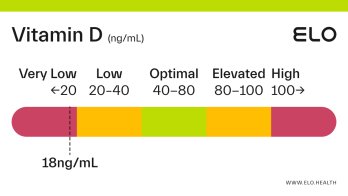
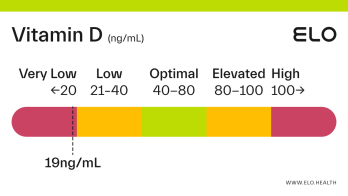
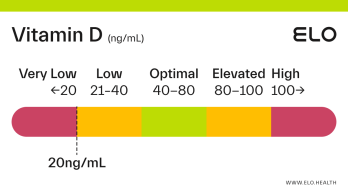
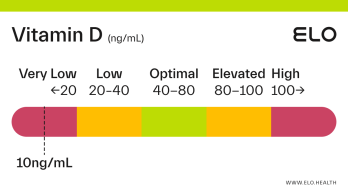
Vitamin D: 10 ng/mL
What does a vitamin D level of 10 mean? Are there any symptoms associated with this vitamin D level?
A vitamin D level of 10 ng/mL is considered severely deficient. Severe deficiency can occur from long-term inadequate intake of vitamin D, limited exposure to sunlight, poor kidney function resulting in impaired conversion of 25(OH)D, or inadequate vitamin D absorption. Prolonged vitamin D deficiency in adults can lead to osteomalacia, a weakening of the bones. Symptoms of osteomalacia include bone deformities and pain, certain types of seizures and spasms, and dental abnormalities.
Low vitamin D may also put you at increased risk for, and severity of COVID-19, diabetes, and cancer. Vitamin D deficiency may also increase your risk for certain autoimmune and neurodegenerative diseases like multiple sclerosis and Alzheimer’s.
Factors that could contribute to a vitamin D level of 10
Diet low in vitamin D
Older age (partly due to a decline in the skin’s ability to synthesize vitamin D with age)
Dark complexion
Living in cold or northern climates (people who live above 37°N latitude cannot synthesize vitamin D year-round)
Limited sun exposure (such as those who spend the majority of their time indoors or are covered when outside)
Pregnancy and breastfeeding
Cystic fibrosis, Crohn's, celiac, kidney, and liver disease, or other conditions that interfere with vitamin D absorption or synthesis
Obesity (greater amounts of subcutaneous fat sequester more of the vitamin)
Gastric bypass surgery
What to do if your vitamin D level is 10?
To improve vitamin D levels:
Increase consumption of vitamin D-rich foods like salmon, herring, canned tuna, eggs (with the yolk), and fortified foods like milk, yogurt, and breakfast cereals
Get 10–30 minutes of unprotected midday sunlight most days
Take a vitamin D supplement. How much you should take depends on your level of deficiency. For a level of 10, you will likely need to take 5,000 IU daily for several months to significantly improve your vitamin D status.
If levels do not improve after 3 months, review your supplements with an expert or talk to your doctor.
Supplements used to improve vitamin D test results
If you are vitamin D deficient, a daily supplement is typically needed to get levels into the optimal range (40-80 ng/mL) over time.
For levels of 10 ng/mL, talk to your healthcare provider. Daily supplementation of vitamin D3 (cholecalciferol) should be considered to achieve adequate body stores of vitamin D.
References
National Institutes of Health. (2021, March 26). Office of Dietary Supplements - Vitamin D. National Institutes of Health – Office of Dietary Supplements.
https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Alshahrani, F., & Aljohani, N. (2013). Vitamin D: deficiency, sufficiency, and toxicity. Nutrients, 5(9), 3605–3616.
https://doi.org/10.3390/nu5093605
Holick M. F. (2009). Vitamin D status: measurement, interpretation, and clinical application. Annals of epidemiology, 19(2), 73–78.
https://doi.org/10.1016/j.annepidem.2007.12.001
Demir, M., Demir, F., & Aygun, H. (2021). Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. Journal of medical virology, 93(5), 2992–2999.
https://doi.org/10.1002/jmv.26832
Kayaniyil, S., Vieth, R., Retnakaran, R., Knight, J. A., Qi, Y., Gerstein, H. C., Perkins, B. A., Harris, S. B., Zinman, B., & Hanley, A. J. (2010). Association of vitamin D with insulin resistance and beta-cell dysfunction in subjects at risk for type 2 diabetes. Diabetes care, 33(6), 1379–1381.
https://doi.org/10.2337/dc09-2321
Examine.com. (2019, April). A D-fence against cancer?
https://examine.com/members/deep-dives/article/a-d-fence-against-cancer/
Yang, C. Y., Leung, P. S., Adamopoulos, I. E., & Gershwin, M. E. (2013). The implication of vitamin D and autoimmunity: a comprehensive review. Clinical reviews in allergy & immunology, 45(2), 217–226.
https://doi.org/10.1007/s12016-013-8361-3