VLDL cholesterol overview

What is the VLDL cholesterol test?
VLDL cholesterol is a test that measures the amount of very-low-density lipoproteins in your blood.
Most labs estimate your VLDL based on your triglyceride level since VLDL particles carry mostly triglycerides through your blood and there is no way to directly measure VLDL. Typically, your VLDL level is about one-fifth of your triglyceride level, but this estimate is less accurate if your triglyceride level is above 400 mg/dL. [ 1 2
What does the VLDL test measure?
This test measures the amount of VLDL (very-low-density lipoproteins) in your blood. Your liver makes VLDL and releases it into your bloodstream. VLDL is similar to LDL cholesterol;
High levels of triglycerides, carried by VLDL particles, create a sticky plaque that narrows artery walls and can contribute to heart attack, stroke, or other health problems. Ideally, your VLDL levels should be less than 30 mg/dL, but lower is better.
What do your VLDL results mean?
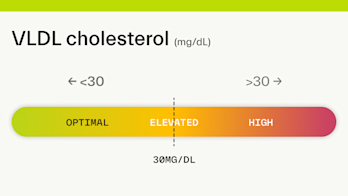
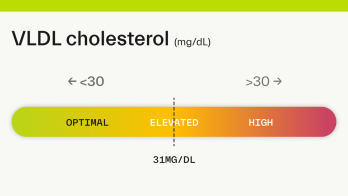
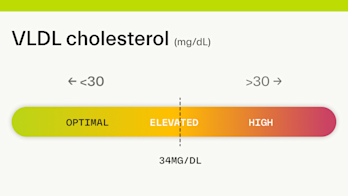
VLDL cholesterol status is classified as follows:
Optimal: <30 mg/dL
Elevated: >30 mg/dL
Optimal results:
Optimal VLDL cholesterol levels are <30 mg/dL. Optimal VLDL cholesterol is associated with better heart health and a lower risk of heart disease.
Elevated results:
Elevated VLDL cholesterol levels are >30 mg/dL. Diet and lifestyle changes can help you decrease your VLDL levels to >30 mg/dL, and lower your risk for coronary artery disease and stroke.
What factors impact VLDL cholesterol levels?
The factors that impact VLDL levels are similar to those that affect triglyceride levels. These include your diet, weight, physical activity level, smoking, and alcohol use. Some medications and certain diseases can also impact triglyceride and VLDL levels.
Diet: Diets that are high in fat, added sugar, and refined carbohydrates can increase VLDL levels.
Weight. Having excess fat, particularly around the abdomen, can also increase VLDL.
Physical Activity. Being active can help lower VLDL levels by lowering your triglycerides.
Medications: Certain medicines can raise your VLDL levels secondary to your triglyceride levels. These include corticosteroids, beta-blockers, thiazide diuretics, antivirals, and estrogen.
Some medical conditions: Diseases involving the thyroid, liver, or kidney, as well as poorly controlled type 2 diabetes can change triglyceride and VLDL levels.
Smoking: Smoking is associated with elevated triglycerides and may also increase VLDL.
Excessive alcohol consumption: Heavy drinking can indirectly increase VLDL levels by raising triglyceride levels.
Groups at risk for high VLDL cholesterol
Individuals with high triglycerides
Those with a diet high in fat, added sugar, and refined carbohydrates
Overweight or obese individuals
Physically inactive adults
Smokers
Alcoholics
Individuals taking certain medications like corticosteroids, beta-blockers, thiazide diuretics, antivirals, and estrogen
Health conditions including hypothyroidism, liver disease, kidney disease, and poorly controlled type 2 diabetes
Diet & lifestyle strategies shown to improve results
The best way to lower VLDL is to reduce your triglycerides [ 3
Exercising for 30-60 minutes 5x/week.
Losing weight.
Avoiding refined carbohydrates and limiting added sugars to less than <25g/day.
Limiting your consumption of alcohol to <1-2 drinks/day.
Eating healthier fats like those found in nuts, seeds, avocados, olive oil, and salmon.
Avoiding trans fats and limiting saturated fat to <10% of total calories.
Quitting smoking.
Medications and supplements used to improve VLDL levels
Medications
If diet and lifestyle changes do not lower triglyceride and VLDL levels enough on their own, some medications and supplements may help.
Prescription niacin: Niacin is a B vitamin that, when taken at prescription doses, can lower VLDL levels by reducing its production in the liver and improving HDL (good) cholesterol levels. [
4
]Fibrates: Help lower high triglyceride levels and may also help raise HDL (good) cholesterol.
Statins: Statins (including atorvastatin, simvastatin, and rosuvastatin) may be prescribed if your LDL and total cholesterol levels are also elevated. Statins reduce cholesterol production in your liver and can effectively reduce VLDL levels [
5
]. Statins are only prescribed if diet and lifestyle changes aren’t enough [6
].
Supplements
Fish oil: The omega-3 fatty acids in fish oil can help lower your triglycerides and therefore reduce VLDL as well. Prescription fish oil contains more active fatty acids than many nonprescription supplements but can interfere with blood clotting, so check with a doctor before taking a high-dose supplement.
References
VLDL Cholesterol. (2019, February 27). MedlinePlus (NIH). Retrieved October 1, 2022, from
https://medlineplus.gov/vldlcholesterol.html
VLDL test. (n.d.). Mount Sinai Health System. Retrieved October 3, 2022, from
https://www.mountsinai.org/health-library/tests/vldl-test
VLDL cholesterol: Is it harmful? (2022, June 17). Mayo Clinic. Retrieved October 3, 2022, from
https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/vldl-cholesterol/faq-20058275
McKenney J. (2004). New perspectives on the use of niacin in the treatment of lipid disorders. Archives of internal medicine, 164(7), 697–705.
https://doi.org/10.1001/archinte.164.7.697
Ginsberg H. N. (1998). Effects of statins on triglyceride metabolism. The American journal of cardiology, 81(4A), 32B–35B.
https://doi.org/10.1016/s0002-9149(98)00035-6
Carotid Artery Disease. (n.d.). National Heart, Lung, and Blood Institute | NIH. Retrieved September 9, 2021, from
https://www.nhlbi.nih.gov/health-topics/carotid-artery-disease
High cholesterol. (n.d.). NHS Inform. Retrieved September 9, 2021, from
https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/high-cholesterol
Cholesterol: Types, Tests, Treatments, Prevention. (2020, July 31). Cleveland Clinic.
https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
Blood Cholesterol | NHLBI, NIH. (2021, January 4). National Institutes of Health.
https://www.nhlbi.nih.gov/health-topics/blood-cholesterol
LDL: The “Bad” Cholesterol. (n.d.). National Institutes of Health. Retrieved September 22, 2021, from
https://medlineplus.gov/ldlthebadcholesterol.html