LDL cholesterol overview

What is a LDL test?
LDL cholesterol is a test that measures the amount of the low-density lipoproteins (“bad cholesterol”) in your blood. Although cholesterol serves several important functions, high LDL cholesterol is a risk factor for heart disease because it sticks to artery walls, leading to plaques.
What does LDL measure?
This test measures the amount of LDL cholesterol in your blood. High levels of LDL create a sticky plaque that narrow arteries and may lead to heart attack, stroke, or other health problems. Ideally, your LDL levels should be less than 100mg/dL, but lower is better.
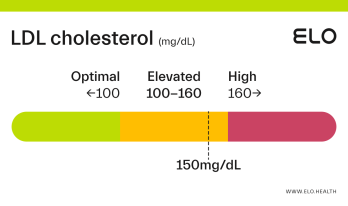
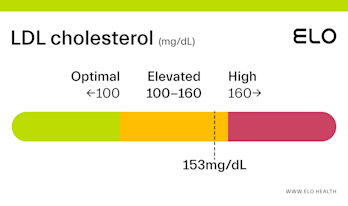
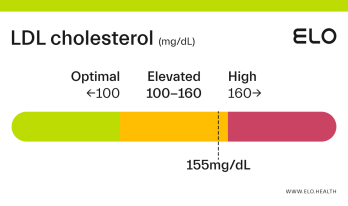
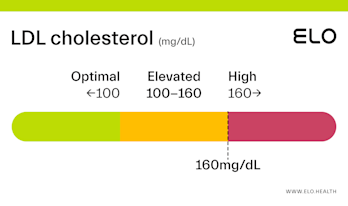
What do your LDL results mean?
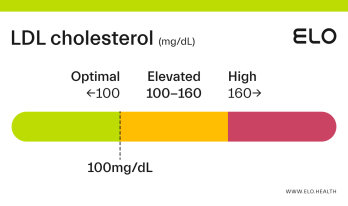
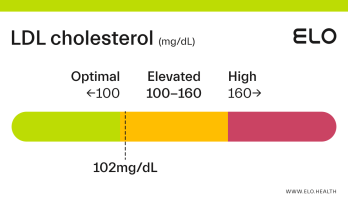
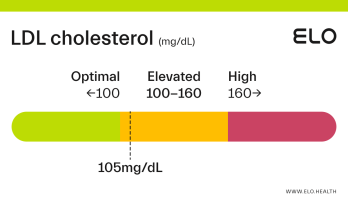
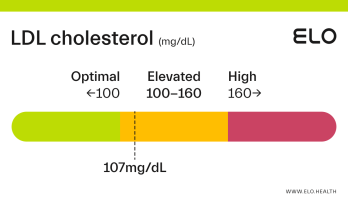
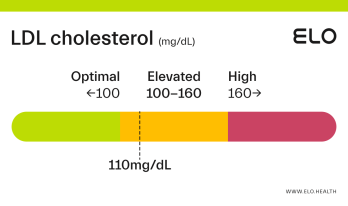
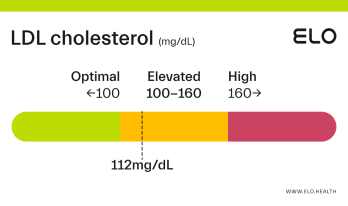
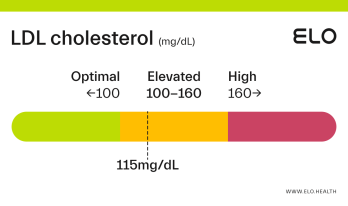
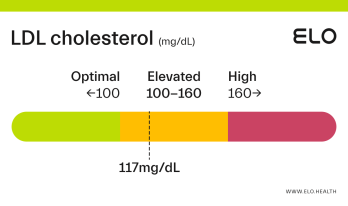
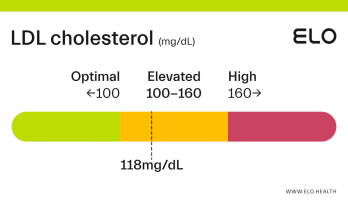
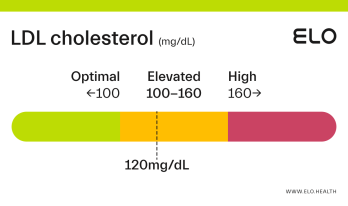
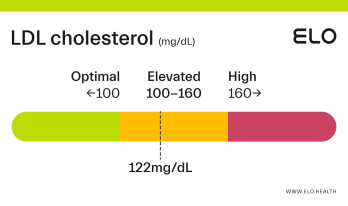
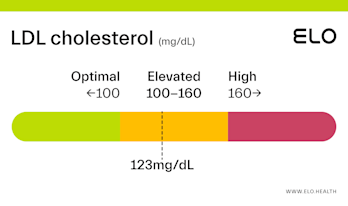
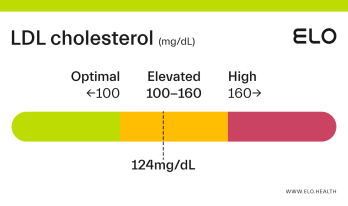
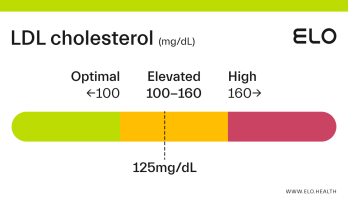
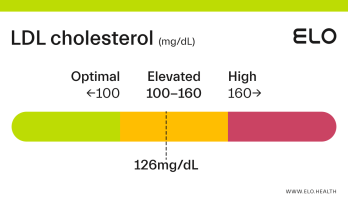
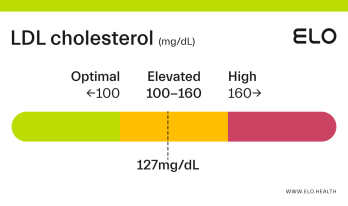
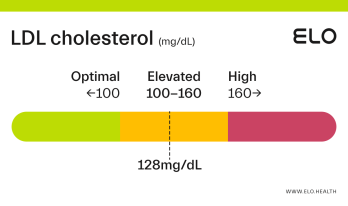
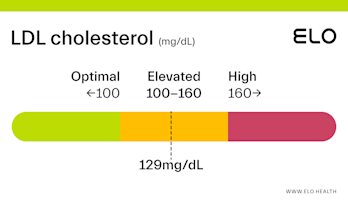
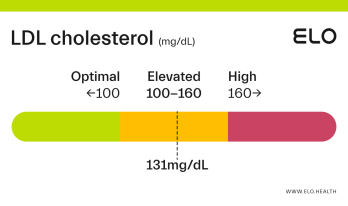
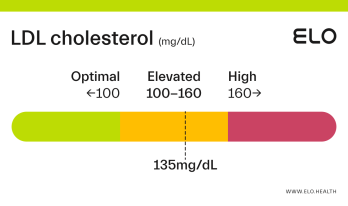
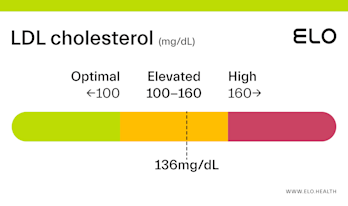
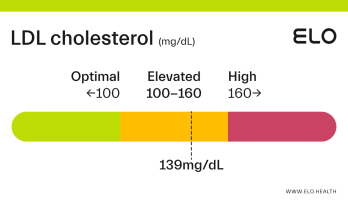
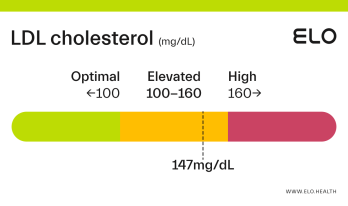
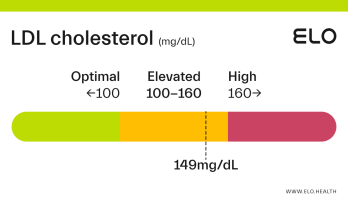
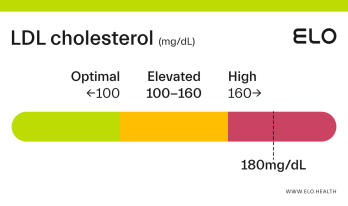
LDL cholesterol status is classified as follows:
Optimal: <100 mg/dL
Elevated: 100-160 mg/dL
High:
>
160 mg/dL
Optimal LDL results:
Optimal LDL cholesterol levels are below 100 mg/dL. Optimal LDL cholesterol is associated with improved heart health and a lower risk of heart disease.
Elevated LDL results:
Elevated LDL cholesterol levels are between 100-160 mg/dL. Diet and lifestyle changes can help you decrease your LDL levels to <100 mg/dL, and lower your risk for coronary artery disease and stroke.
High LDL results:
LDL cholesterol levels above 160 mg/dL are considered high. High LDL cholesterol is associated with an increased risk of heart attack, stroke, and sudden cardiac arrest [2]. If your LDL cholesterol is high, diet and lifestyle can help reduce your levels back into the elevated or optimal range. Some people may also need to take a cholesterol-lowering medication.
While high cholesterol is typically tied to diet and lifestyle factors, familial hypercholesterolemia (FH) can also cause high cholesterol levels. FH is a common genetic disorder that causes LDL cholesterol to increase. If untreated, FH can lead to early heart attacks and heart disease in even young adults and children. Because FH is inherited, when one family member is diagnosed, it’s important all family members are also screened for this condition.
What factors impact LDL cholesterol levels?
A variety of factors can affect LDL levels including your diet, weight, physical activity level, and whether or not you smoke. Medications, certain diseases, as well as your age, sex, race, and genetics also impact LDL levels.
Diet: Diets that are high in saturated fats, trans fats, added sugar, and low in fiber can increase LDL levels.
Weight. Having excess fat, particularly around the abdomen, can also increase LDL cholesterol.
Physical Activity. Being active can help lower “bad” LDL cholesterol levels, and raise “good” HDL cholesterol levels..
Smoking. Smoking lowers your HDL cholesterol which can contribute to a higher level of LDL cholesterol.
Medications: Certain medicines can raise your LDL level. including corticosteroids, beta-blockers, thiazide diuretics, antivirals, retinoids, and growth hormones.
Some medical conditions: Diseases such as chronic kidney disease, diabetes, and HIV/AIDS can cause a higher LDL level.
Age and Sex: LDL cholesterol levels tend to increase with age in both men and women. Women tend to have lower LDL levels than men, but their levels typically go up after menopause.
Genetics (heredity): Family members often have similar cholesterol levels, which suggests your genes can raise your risk of having unhealthy cholesterol levels.
Race. Some races are at greater risk of high LDL cholesterol. For example, Blacks/African Americans typically have higher LDL than Caucasians [8].
Groups at risk for high LDL
Those with a diet high in saturated fats, trans fats, and added sugar, and with low fiber intake
Overweight or obese individuals
Physically inactive adults
Smokers
Individuals taking certain medications like corticosteroids, beta-blockers, thiazide diuretics, antivirals, retinoids, and growth hormones
Those with a family history of high LDL/ low HDL cholesterol, heart disease, heart attack, and/or stroke
Certain health conditions including chronic kidney disease, diabetes, and HIV/AIDS
Diet & lifestyle strategies shown to improve LDL results
To lower LDL cholesterol levels:
Be active every day: Aim for 30-60 minutes of physical activity 5x/week.
Eat fiber-rich foods such as veggies, fruit, whole grains, and legumes, daily for a total of 30-40g fiber/ day.
Limit sources of refined carbs and added sugars such as soda, chips, candy, baked goods, sweetened yogurt, and ice cream.
Eat small, fatty fish such as salmon, sardines, and trout, at least twice a week.
Incorporate plant sterols and stanols daily (2g) in the form of food or a supplement.
Avoid trans fats (partially hydrogenated oils) and reduce saturated fat intake to < 10% total calories.
Quit smoking.
Medications and supplements used to improve LDL results
Medications
Medications are typically prescribed if diet and lifestyle changes do not lower LDL cholesterol levels enough on their own. Some common cholesterol medications include:
Statins: Statins (including atorvastatin, simvastatin, and rosuvastatin) reduce cholesterol production in your liver. Because they typically need to be taken for life, statins are only prescribed if diet and lifestyle changes aren’t enough [3].
Ezetimibe can be helpful for those with familial hypercholesterolemia and/or who have side effects with statins.
Bile acid sequestrants: These medications block cholesterol-rich bile acid from being absorbed into the bloodstream and can be prescribed in place of or in addition to a statin.
PCSK9 inhibitors: This medicine is injected under your skin every 2 or 4 weeks and may be prescribed alongside a statin if you are at high risk of heart attack or stroke, or have familial hypercholesterolemia.
Lomitapide: Typically prescribed if you have familial hypercholesterolemia and requires liver enzyme monitoring as it can cause liver damage. Lomitapide is commonly also taken with vitamin E.
Supplements
Plant sterols and stanols: Found in plant cell membranes, plant sterols and stanols (also called phytosterols) are similar in structure to cholesterol in the body and block dietary cholesterol from being absorbed. Phytosterols can be found in small quantities in vegetable oils, nuts, legumes, whole grains, fruits, and vegetables, however, the average daily intake (500 mg) is typically not enough to lower cholesterol. Studies show consuming 2000 mg (2 g) of plant sterol and stanols daily from diet and/or supplements to be most effective [4]. Plant sterol and stanol supplements are taken before or with meals can help lower total cholesterol in parallel with other recommended diet and lifestyle changes [4].
Beta-glucan: Beta-glucan is a form of soluble fiber that has been shown to help lower cholesterol levels. It’s found naturally in whole grains like barley, oats, rye, and wheat, mushrooms, and seaweed, and is also available as a nutritional supplement. For cholesterol-lowering benefits, consume 3-7 g/day from your diet and/or a supplement.
Psyllium: Another type of soluble fiber made from the husk of psyllium seeds, psyllium is good for digestive health and regularity, and can also be helpful in lowering cholesterol. Psyllium supplements are sold in powder form and can help reduce lipid levels when taken daily at a dose of 8-12g/day.
Alpha-lipoic acid: A potent antioxidant made in the body, alpha lipoic acid is also found in foods including carrots, beets, spinach, broccoli, potatoes, and red meat. Research indicates that 600 mg/day of alpha-lipoic acid from your diet and/or a supplement may help lower total cholesterol and LDL (bad) cholesterol [8].
Bergamot extract: Bergamot is a citrus fruit that has long been used for medicinal purposes. Taking bergamot extract (made from the juice of the fruit) seems to lower cholesterol and triglyceride levels in adults with high cholesterol [9,10]. One study suggests taking bergamot extract daily for a month may be as effective as taking a low dose of the cholesterol-lowering drug called rosuvastatin (Crestor) [10]. A recent research review indicates that 1000 mg/day may be most effective for lowering cholesterol.
Green tea extract: Made from the leaves of the Camellia sinensis plant, green tea extract is a natural supplement that has been shown to help lower LDL (bad) and total cholesterol [11]. A daily dose of 400 mg may help lower your cholesterol but check with your doctor first as green tea extract can interact with certain medications, including beta-blockers and blood thinners. In addition, green tea extract may also have a stimulant effect.
Berberine: A compound extracted from a variety of medicinal herbs, some studies suggest berberine can reduce LDL (bad) cholesterol and triglycerides in type 2 diabetics, as well as slightly increase HDL (good) cholesterol [12]. The standard dose of berberine is 900-2000 mg/day (divided into 3-4 doses), taken with or just after a meal.
References
Cholesterol Levels: What You Need to Know. (n.d.). U.S. National Library of Medicine | NIH. Retrieved September 9, 2021, from
https://medlineplus.gov/cholesterollevelswhatyouneedtoknow.html
Carotid Artery Disease. (n.d.). National Heart, Lung, and Blood Institute | NIH. Retrieved September 9, 2021, from
https://www.nhlbi.nih.gov/health-topics/carotid-artery-disease
High cholesterol. (n.d.). NHS Inform. Retrieved September 9, 2021, from
https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/high-cholesterol
Racette, S. B., Lin, X., Lefevre, M., Spearie, C. A., Most, M. M., Ma, L., & Ostlund, R. E., Jr (2010). Dose effects of dietary phytosterols on cholesterol metabolism: a controlled feeding study. The American journal of clinical nutrition, 91(1), 32–38.
https://doi.org/10.3945/ajcn.2009.28070
Cholesterol: Types, Tests, Treatments, Prevention. (2020, July 31). Cleveland Clinic.
https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
Blood Cholesterol | NHLBI, NIH. (2021, January 4). National Institutes of Health.
https://www.nhlbi.nih.gov/health-topics/blood-cholesterol
LDL: The “Bad” Cholesterol. (n.d.). National Institutes of Health. Retrieved September 22, 2021, from
https://medlineplus.gov/ldlthebadcholesterol.html
Mousavi, S. M., Shab-Bidar, S., Kord-Varkaneh, H., Khorshidi, M., & Djafarian, K. (2019). Effect of alpha-lipoic acid supplementation on lipid profile: A systematic review and meta-analysis of controlled clinical trials. Nutrition (Burbank, Los Angeles County, Calif.), 59, 121–130.
https://doi.org/10.1016/j.nut.2018.08.004
Cai, Y., Xing, G., Shen, T., Zhang, S., Rao, J., & Shi, R. (2017). Effects of 12-week supplementation of Citrus bergamia extracts-based formulation CitriCholess on cholesterol and body weight in older adults with dyslipidemia: a randomized, double-blind, placebo-controlled trial. Lipids in health and disease, 16(1), 251.
https://doi.org/10.1186/s12944-017-0640-1
Gliozzi, M., Walker, R., Muscoli, S., Vitale, C., Gratteri, S., Carresi, C., Musolino, V., Russo, V., Janda, E., Ragusa, S., Aloe, A., Palma, E., Muscoli, C., Romeo, F., & Mollace, V. (2013). Bergamot polyphenolic fraction enhances rosuvastatin-induced effect on LDL-cholesterol, LOX-1 expression and protein kinase B phosphorylation in patients with hyperlipidemia. International journal of cardiology, 170(2), 140–145.
https://doi.org/10.1016/j.ijcard.2013.08.125
Xu, R., Yang, K., Li, S. et al. Effect of green tea consumption on blood lipids: a systematic review and meta-analysis of randomized controlled trials. Nutr J 19, 48 (2020).
https://doi.org/10.1186/s12937-020-00557-5
Berberine, Examine. (2021, May 5). Examine.com.
https://examine.com/supplements/berberine/#