HbA1c overview

What is an A1c test?
The HbA1c (Hemoglobin A1c) test is a blood test that measures your average blood sugar level over the last 2-3 months.
What does an A1c test measure?
When sugar (glucose) builds up in your blood, it binds to a protein called hemoglobin in your red blood cells. HbA1c measures how much glucose is bound to your red blood cells. Specifically, HbA1c reflects the percentage of your red blood cells that have sugar-coated hemoglobin.
HbA1c is most often used to diagnose pre-diabetes and diabetes and monitor the effectiveness of interventions to manage blood sugar. Symptoms of pre-diabetes and diabetes often can go undetected, and it’s beneficial to know your A1c level even if you’re not at high risk for developing these conditions.
What do your A1c results mean?
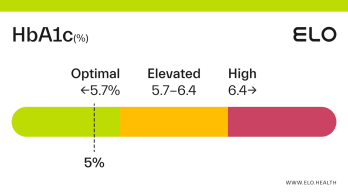
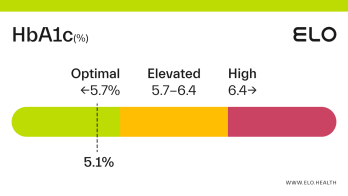
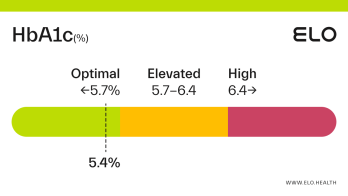
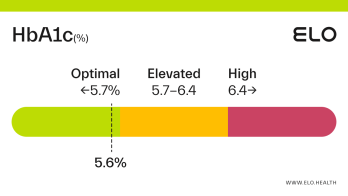
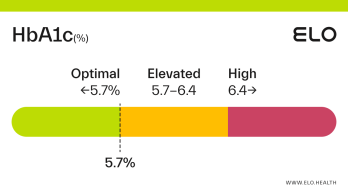
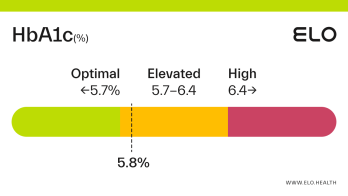
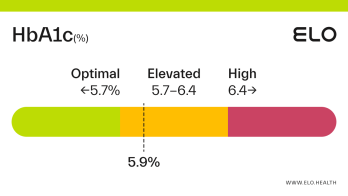
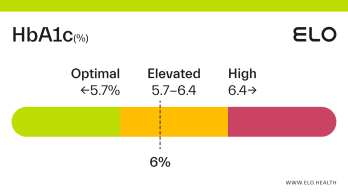
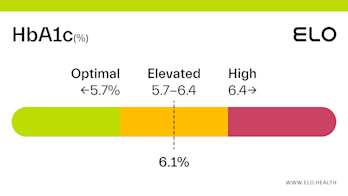
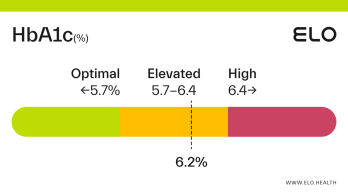
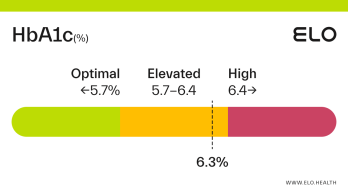
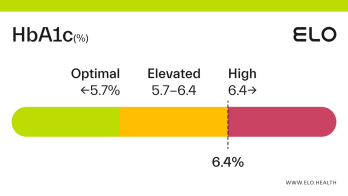
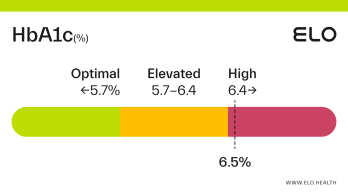
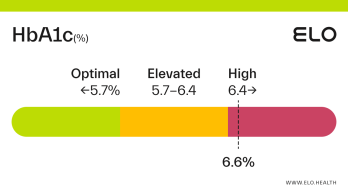
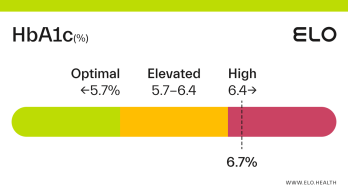
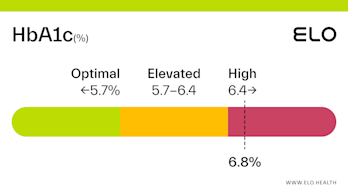
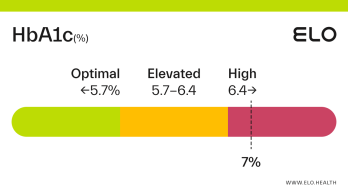
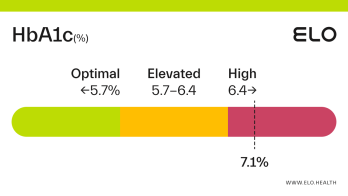
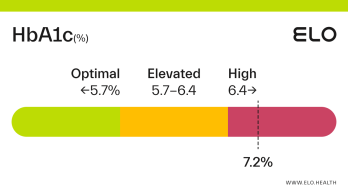
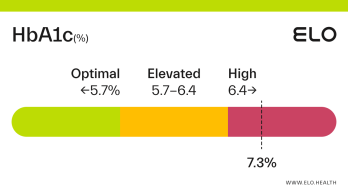
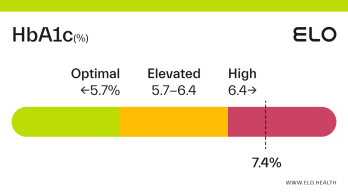
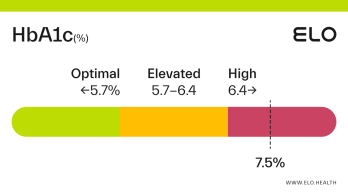
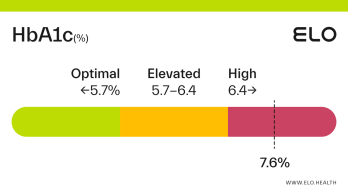
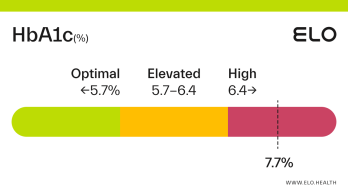
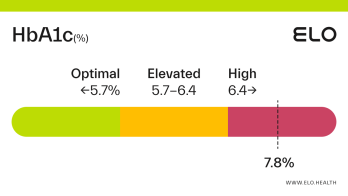
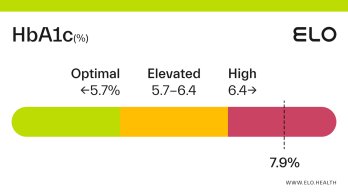
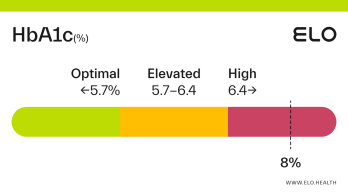
HbA1c status is classified as follows:
Optimal: <5.7%
Elevated: 5.7-6.4%
High:
>
6.5%
Optimal A1c results:
Optimal A1c levels are below 5.7%. For people without diabetes, the normal range for hemoglobin A1c is between 4% and 5.6%.
Elevated A1c results:
You have elevated A1c if your level is between 5.7-6.4%. Elevated A1c is considered prediabetes. If your A1c is elevated, diet and lifestyle changes may be effective for getting your levels back into the optimal range without the need for medications. Prediabetes raises your risk of type II diabetes, heart disease, and stroke, and taking action to reduce your A1c level can have a significant impact on your health.
High A1c results:
A1c levels
>
6.5% are considered high. If you have an A1C level greater than 6.4%, your levels are in the diabetes range. Diabetes occurs when the body doesn’t use insulin properly, causing sugar to build up in the blood which puts you at greater risk for certain health problems. Some people can control their blood sugar levels with healthy eating and exercise, while others may need medication or insulin to help manage it. Having diabetes raises your risk of heart disease, stroke, kidney disease, visual impairment, neuropathy, and various other conditions.What factors impact A1c levels?
A variety of factors can affect A1c levels. These include:
Diet, particularly those high in refined carbohydrates and added sugars, and low in fiber
Overweight/ obesity
Sedentary lifestyle
Age
Race (people of Black, Hispanic/Latino, American Indian, Asian American, or Pacific Islander descent are at greater risk for prediabetes/ diabetes.)
Stress
Certain medications, including glucocorticoids
Genetics (family history of pre-diabetes or diabetes)
Adherence to your prediabetes/ diabetes management plan
Pregnancy
Chronic disease/ inflammation
Several things can also falsely increase or decrease your A1c result. These include:
Kidney failure, liver disease, or severe anemia
Certain medicines, including opioids and some HIV medications
Blood loss or blood transfusions
Early or late pregnancy
A less common type of hemoglobin found in people of African, Mediterranean, or Southeast Asian descent, as well as people with blood disorders like sickle cell anemia or thalassemia
Let your doctor know if any of these apply to you to determine if you need follow-up testing.
Groups at risk for high A1c
Certain people are at greater risk for having elevated A1c and are therefore at greater risk for prediabetes and diabetes. These include [2]:
Adults age 45 or older
People of Black, Hispanic/Latino, American Indian, Asian American, or Pacific Islander descent
Individuals with a parent, brother, or sister with diabetes
Overweight or obese individuals
Those who are physically inactive
Individuals with low HDL (good) cholesterol and/or high triglycerides
People with high blood pressure, or who take medicine for high blood pressure
Women who had diabetes during pregnancy or who have been diagnosed with polycystic ovary syndrome (PCOS)
Diet & lifestyle strategies shown to improve A1c results
Making changes to your diet and adopting healthier habits can help lower your HbA1c. To lower your HbA1c level:
Be active every day: Aim for 150 minutes of moderate physical activity per week (about 30 minutes, 5 days per week).
Aim for half a plate of non-starchy veggies at every meal, and incorporate a source of lean protein and plant-based fat to assist with blood sugar control.
Limit refined carbohydrates and added sugar, and choose whole-grain carbohydrates such as whole wheat bread/ pasta, quinoa, farro, and steel-cut oats, instead.
Lose excess weight if you are overweight or obese.
Follow your diabetes treatment plan if you have been diagnosed with diabetes.
Manage stress and get adequate sleep.
Medications used to improve A1c results
Medications can be helpful to lower elevated A1c levels into a safer range if diet and lifestyle modifications aren’t sufficient. Some common diabetes medications include:
Insulin: Typically given by injection or through a pump to increase glucose (sugar) uptake by cells and thus decrease blood sugar levels.
Sulfonylureas: Reduce blood glucose by stimulating insulin-producing beta cells in the pancreas and increasing insulin levels.
Alpha-glucosidase inhibitors: Help your body break down starches and sugars found in food which, in turn, lowers blood sugar levels.
Biguanides: Makes your body more sensitive to insulin by decreasing the amount of sugar produced by your liver, as well as how much sugar your intestines absorb. The most common biguanide is metformin.
Dopamine agonist: Work by affecting the way the brain processes dopamine, an important neurotransmitter (chemical messenger). By increasing the activity of dopamine receptors, dopamine agonists increase insulin sensitivity, allowing cells to use blood glucose more effectively and lower blood sugar.
DPP-4 inhibitors: Help your body continue to make insulin, which lowers blood sugar.
GLP-1 receptor agonists: Lower blood sugar by increasing growth of insulin-producing beta-cells in the pancreas, slowing stomach emptying, and decreasing appetite.
Meglitinides: Similar to sulfonylureas (but by a different mechanism) meglitinides stimulate the pancreas to release insulin in response to a meal. This increase in insulin production helps lower blood sugar.
SGLT 2 inhibitors: Prevent the kidneys from holding on to glucose and increasing glucose excretion in urine.
Thiazolidinediones: Decreases glucose in your liver and helps your fat cells better utilize insulin.
References
All About Your A1C. (2018, August 21). Centers for Disease Control and Prevention.
https://www.cdc.gov/diabetes/managing/managing-blood-sugar/a1c.html
Diabetes Risk - What Causes Diabetes. (n.d.). American Diabetes Association. Retrieved September 14, 2021, from
https://www.diabetes.org/diabetes-risk
Cherney, K. (2020, June 18). A Complete List of Diabetes Medications. Healthline.
https://www.healthline.com/health/diabetes/medications-list